Also see:
Ray Peat, PhD on Low Blood Sugar & Stress Reaction
PUFA Promote Stress Response; Saturated Fats Suppress Stress Response
Protect the Mitochondria
Saturated and Monousaturated Fatty Acids Selectively Retained by Fat Cells
PUFA Decrease Cellular Energy Production
The Randle Cycle
Low Carb Diet – Death to Metabolism
Free Fatty Acid Suppress Cellular Respiration
Blood Sugar – Resistance to Allergy and Shock
Sugar (Sucrose) Restrains the Stress Response
Protection from Endotoxin
Possible Indicators of High Cortisol and Adrenaline
Thyroid peroxidase activity is inhibited by amino acids
Toxicity of Stored PUFA
Belly Fat, Cortisol, and Stress
Sugar (Sucrose) Restrains the Stress Response
A long childhood feeds the hungry human brain
“Every stress leaves an indelible scar, and the organism pays for its survival after a stressful situation by becoming a little older.” -Hans Selye
“Since glucose is the main fuel for the brain, and since the human brain is the factor that elevates man above other animals, mother nature took special precautions against a lack of glucose in the bloodstream at all times.” -Broda Barnes & Charlotte Barnes
“In other words, the thyroid has a profound effect on the liver. We have other evidence that a lack of thyroid is accompanied by a sluggish liver…Since a sluggish liver is the most common cause of hypoglycemia, it should follow that the hypothyroid patient is highly susceptible to low blood sugar.” -Broda Barnes, MD, PhD and Charlotte Barnes
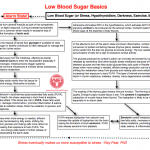
The flow chart thumbnail below is inspired by the work of Ray Peat, PhD and attempts to identify the major players involved in the regulation of blood sugar in the event of hypoglycemia. The alarm or stress reaction that occurs during low blood sugar is a lifesaver during actual starvation or when we can’t get to food, but it should ideally only turn on occasionally.
The more we enter survival (alarm) mode, the greater the pituitary and adrenal activity become dominant relative to thyroid activity. If the blood sugar is chronically low due to illogical food choices or imbalanced or infrequent meals, the alarm state is active too frequently and problems develop over time.
The heightened sympathetic nervous system activity during low blood sugar is like that which happens in hypothyroidism & during prolonged darkness, exercise, and malnutrition. The interconnectedness of the stress mediators is significant since they tend to promote each other in vicious, self-accelerating loops especially when the tissues are rich in polyunsaturates, if the bowel is toxic, or in a backdrop of low carbon dioxide or high estrogen.
The response to stress changes with age in relation to our previous dietary choices. In youth (assuming an adequate diet), the relative deficiency of stored unsaturates, high thyroid, glycogen availability, and optimal protective steroid hormone production produces a self-limiting stress response instead of a self-stimulating one.
As the tissues become more unsaturated with aging or due to poor food choice, the stress response switches from adaptive to dysadaptive, making the body progressively less capable of handling future stresses without producing inflammation and other adverse effects. The unsaturates’ anti-thyroid actions slow the synthesis of protective steroid hormones (pregnenolone, DHEA, progesterone) from cholesterol; cortisol becomes the dominant stress steroid and the ratio of cortisol to testosterone & estrogen to progesterone increases.
Using multiple means, the body protectively slows the metabolism (goes into economy mode) during stress to prolong survival since the body consumes itself during such times. This effect is favorable if you’re actually starving and food isn’t available but not friendly if long-term weight management is desired. Immune function is also suppressed, making the body more susceptible to infection and sickness.
The ability to store enough glycogen to handle stress lessens the need for adrenal activity. With thyroid suppression comes less ability to store glycogen, making low blood sugar and the alarm state more common. Without an energized liver, the conversion of T4 to T3 becomes less efficient, increasing adrenal and pituitary activity. An increased dependence on cortisol to provide glucose for fuel results, wasting protein rich-tissues like skeletal muscle. The loss of muscle tissue (and bone mass) is a characteristic of aging.
As the thyroid activity is suppressed, liver function suffers allowing estrogen to accumulate. Estrogen further blocks thyroid function, depletes glycogen, increases fatty acids, amplifies endotoxin’s effects, is toxic to the liver, and promotes inflammation in another cruel cycle.
Blood sugar balance using protective and digestible food choices is a fundamental of good nutrition practices. While some will argue that we don’t need to eat carbohydrate because our body can make carbohydrate from itself, that side of the fence is looking at physiology through a pin hole and misses the big picture. Ample carbohydrate particularly from ripe fruits, orange juice, milk, honey, and sucrose keeps the alarm state and vicious inflammatory cycles at bay.
The body uses its own tissues to make glucose during hypoglycemia because glucose is important in maintaining optimal function. Without enough dietary carbohydrate, the body becomes dependent on stress hormones for glucose. For optimal health, sustain blood sugar with food, not stress hormones.
The sympathetic nervous system is associated with fight or flight. The parasympathetic side relates to rest and digestion. Excessively sympathetic stimulation degrades digestive (and reproductive) function and sleep quality. The often ignored portion of the low blood sugar puzzle is the effects of poor circulation on the intestines as blood flow shifts to the muscles and brain during fight or flight and away from the digestive tract.
The de-energized intestines not only allow intestinal toxins into the blood stream more easily as barrier function is compromised, but the digestion of foods becomes less efficient also leading to malnutrition. The increased endotoxin exposure triggers inflammation in a multitude of ways along with edema, suppression of oxidation metabolism & detoxification, and a rise in free fatty acids & estrogen.
Hypothyroidism, exercise, and low blood sugar increase fight or flight activity, promoting the loss of carbon dioxide (CO2). If you think of carbon dioxide as a waste product of cellular respiration, then this might not seem like a big deal. However, carbon dioxide is anything but a waste product. A more accurate description labels CO2 as the hormone of cellular respiration since it has many protective & stabilizing functions.
Inhabitants of high altitude regions have longer lifespans and decreased susceptibility to disease relative to low altitude populations suggesting that carbon dioxide is of major importance to our physiology. Excessive CO2 loss from hyperventilation during stress perpetuates the alarm state and increases another mediator of stress, lactic acid, as cells begin producing energy without oxygen because of a lack of CO2 (Bohr Effect).
One of the interesting characteristics of the stress response is that in some circumstances the free fatty acids liberated by adrenaline (and other lipolytic stress substances) can block the glucose produced by cortisol’s action from being used (glucose-fatty acid cycle or Randle Cycle) by cells. This competitive inhibition could appear as high blood sugar on a lab test and a deficiency of insulin would be suspected by white coated professionals, but the elevated free fatty acids from the alarm state are the problem.
During a time of stress when more energy is needed, efficient energy production can be blocked by fatty acids, shifting the metabolism away from glucose and making cells more reliant on fats for energy, increasing their exposure to toxic PUFA. Damage to the cells’ power factory, the mitochondrion, occurs and carbon dioxide & steroid hormone production falls. This type of internal environment is a precipitating factor in insulin resistance, diabetes, obesity, many degenerative conditions, and aging.
By simply balancing the blood sugar with appropriate food choices and avoiding excessive stimulation, much can be done to flip from degeneration & inflammation into regeneration. Taking steps to eliminate the consumption of food rich in polyunsaturates is a protective dietary measure. Niacinamide, vitamin E, aspirin, red light, ample dietary carbohydrate & sodium, and saturated fats are easily introduced therapies that protect us from already stored polyunsaturates.

Very good article.
I disagree with this point in the article. People who experience blood sugar swings that send them into hypoglycemia should avoid quick digesting carbohydrates. That is precisely how they got into the position they are in. That’s just horrible advice.
“While some will argue that we don’t need to eat carbohydrate because our body can make carbohydrate from itself, that side of the fence is looking at physiology through a pin hole and misses the big picture. Ample carbohydrate particularly from ripe fruits, orange juice, milk, honey, and sucrose keeps the alarm state and vicious inflammatory cycles at bay.”
The scenario you predict is more likely to occur from eating a starch or from eating protein alone. The glycemia of the carbohydrates I listed is moderate and all but sucrose comes with beneficial micronutrients as well, but even sucrose is beneficial.
J Neuroendocrinol. 2001 Sep;13(9):827-35.
A new perspective on glucocorticoid feedback: relation to stress, carbohydrate feeding and feeling better.
Laugero KD.
Sugar (Sucrose) Restrains the Stress Response
http://www.functionalps.com/blog/2011/02/04/sugar-sucrose-restrains-the-stress-hormone-system/
The fructose component of the listed foods (outside of milk). Milk is unique though since it contains protein, fat, and carbohydrate making it a balanced meal and a logical recommendation.
Diabetes Care. 1982 Sep-Oct;5(5):512-7.
The effects of oral fructose, sucrose, and glucose in subjects with reactive hypoglycemia.
Crapo PA, Scarlett JA, Kolterman OG, Sanders LR, Hofeldt FD, Olefsky JM.
Thumbs Up: Fructose
http://www.functionalps.com/blog/2012/02/03/thumbs-up-fructose/
I think my issue with this is the medium through which glucose arrives in the body. I am partial with achieving satiety through adequate fat and protein first which helps prevent over consumption of the carbs that can cause hypoglycemia in the first place. Adequate fat/protein first provide satiety and satiation while slower digesting carbohydrate is used to balance out the need for glucose at a steady rate. Patching the blood sugar dysregulation with more high glycemic sugar foods seems to me to be a remedial solution. However I do agree that certain fruits/veggies higher in fiber and lower in sucrose have a good contribution to repairing broken mechanisms. Like you say, a balanced meal… I have looked at some baboon and monkey documentaries and studies and the majority of the stress in these hierarchical “tribes” is induced from the top down in hierarchy. The stress response shows up more in the lower members of the family irrespective of food consumed. I think one would almost have to isolate the dominant monkey and deprive them of fruit to truly understand the sucrose deprivation effect…however I’m only babbling at this point. Thanks for the reply.
This article makes sense of a lot of my symptoms, thank you. I have stress hormone attacks when I take a 1mg prednisone tablet (for my rheumatoid arthritis – am weaning off slowly). These make me feel like I have sudden low blood sugar and make me feel suddenly very weak, listless and I breathe too fast and twitch involuntarily. Taking a teaspoon of sugar brings me out of it quite quickly nowadays, whereas these episodes used to last upwards of half an hour, now I am down to just 5 minutes or so. It seems that in me the addition of cortisol (in pill form) triggers a stress hormone cascade. After having been on steroids for the past 10 years, it seems they are now responsible for stress, rather than helping me to handle it, counterintuitively. I have been supplementing with progest e for the past six months which has reduced my stress hormone response markedly, helped my digestion, increased my CO2 levels (along with buteyko breathing) and made me feel much calmer and happier overall. I have also slowly been shifting my diet away from PUFAs to saturated fats, though this is the hardest part in my view as there are so many hidden fats. Your articles have helped me so much to understand what is going on inside me and to reduce my inflammation and stress hormones and regain some control of my debilitating symptoms, thank you!