Also see:
Ray Peat, PhD on Thyroid, Temperature, Pulse, and TSH
Thyroid Status and Cardiovascular Disease
Protect the Mitochondria
PUFA Promote Cancer
The Cholesterol and Thyroid Connection
High Blood Pressure and Hypothyroidism
A Cure for Heart Disease
Hypothyroidism and A Shift in Death Patterns
The Truth about Low Cholesterol
Thyroid Status and Oxidized LDL
Inflammatory TSH
“Normal” TSH: Marker for Increased Risk of Fatal Coronary Heart Disease
PUFA Decrease Cellular Energy Production
Free Fatty Acids Suppress Cellular Respiration
PUFA Breakdown Products Depress Mitochondrial Respiration
“Curing” a High Metabolic Rate with Unsaturated Fats
Fat Deficient Animals – Activity of Cytochrome Oxidase
PUFA and Liver Toxicity; Protection by Saturated Fats
Unsaturated Fats and Heart Damage
“In the last 20 years, there have been many studies showing that lowering cholesterol increases mortality, especially from cancer and suicide, and that people with naturally low cholesterol are more likely to die from cancer, suicide, trauma, and infections than people with normal or higher than average cholesterol.” -Ray Peat, PhD
“There’s almost no context in which I would speak of “an appropriate dose of T4,” since thyroxin is so effective as an antithyroid substance. It’s appropriate if you are also taking T3, or if you want to shrink your thyroid. Thyroid will dependably correct your pregnenolone production, if you have enough cholesterol, vitamin A, and protein. The cholesterol will be consumed to make pregnenolone and progesterone and bile acids. If cholesterol is below 160, fruit sugar helps to raise it. The protein is needed to detoxify estrogen, unsaturated oils, etc, and to maintain the T3. Protein deficiency gives antithyroid signals, and T4 will be used to make reverse T3 to inhibit T3’s effects. About 3 mcg of T3 especially if it’s taken with milk or gelatine-rich salty soup is effective for stopping the nocturnal alarm reaction.” -Ray Peat, PhD
“In other words, the thyroid has a profound effect on the liver. We have other evidence that a lack of thyroid is accompanied by a sluggish liver. In the first place, it has been apparents for a century that patients with myxedema (very low thyroid activity) have a yellowish tint to their skins. This has been found to be due to the presence of too much carotene in the blood. The liver converts carotene into vitamin A which is colorless. Under the administration of thyroid, the liver becomes more active and the carotene soon disappears. In the second place, the cholesterol level in the blood sis usually elevated in hypothyroidism. Thyroid administration will lower cholesterol, and if too much is given, the cholesterol will fall below normal. The liver converts cholesterol into bile salts which are eliminated in the bile; this process is the usual means of eliminating excess cholesterol. The liver is sluggish in this function among thyroid-deficient individuals…Since a sluggish liver is the most common cause of hypoglycemia, it should follow that the hypothyroid patient is highly susceptible to low blood sugar.” -Broda Barnes, MD, PhD and Charlotte Barnes
“The supply of cholesterol, thyroid and vitamin A must always be adequate for the production of steroid hormones and bile salts. When stress suppresses thyroid activity, increased cholesterol probably compensates to some extent by permitting more progesterone to be synthesized.” -Ray Peat, PhD
“A person may have normal levels of thyroxin but not be converting it adequately to the active form of the thyroid hormone (triiodothyronine or liothyronine). High cholesterol is practically diagnostic of hypothyroidism. Why? Because thyroid hormone controls the conversion of cholesterol to important anti-aging hormones and to bile salts. However, many hypothyroid people have low cholesterol from a suppressed immune system, liver problems, or from eating a low protein (vegan) diet.” -Lita Lee, PhD
By 1930 a clear relationship between thyroid hormone and cholesterol had been established. High cholesterol was formerly used as a reliable marker for hypothyroidism. Much of what we have learned about human and animal physiology continues to be blurred by marketing, special interest, existing pharmaceutical patents, and the pursuit of mega profits.
When billions of dollars are at stake, it’s easy to have amnesia regarding cholesterol’s important role in human and animal physiology. The medical culture has done an exceptional job of firmly ingraining the idea that cholesterol is bad and the lower the serum cholesterol the better off you are. However, this anti-cholesterol sentiment isn’t warranted and such a stance is ignorant and harmful.
Cholesterol
Despite being widely villainized, cholesterol is a protective substance and plays an important role in our physiology. Most cholesterol is not obtained from food but is manufactured endogenously by the the liver. Cholesterol serves two relevant functions as it applies to our discussion – it acts as the raw material for both bile salts and steroid hormones.
Bile salts are made from cholesterol in the liver and stored in the gallbladder. The entry of dietary fats into the small intestine signals the release of bile from the gallbladder through the common bile duct into the small intestine. Bile salts serve two major functions:
(1) excretion of fat-soluble toxins, bilirubin, and excess cholesterol
(2) transportation and absorption of dietary fats
Steroid hormones are made in multiple tissues from LDL cholesterol. These hormones include DHEA, pregnenolone, and progesterone as well as aldosterone, cortisol, testosterone, and the estrogens. Each of these substances plays a multi-faceted role in our physiology, and the inability to convert LDL cholesterol to these protective steroids and bile salts can produce detrimental effects if left uncorrected over a long period of time.
Liver and Thyroid
The liver performs many functions and its health is paramount to ridding the body of toxins, regulating blood sugar & estrogen, producing cholesterol, and supporting metabolism. The thyroid gland in located in the lower front portion of your neck and is responsible for making thyroid hormones that regulate metabolism and energy.
Most of the hormone that the thyroid gland itself makes is a precursor hormone, known as T4 or thyroxine. T4 does NOT increase the metabolism; it must be converted into another hormone, T3 or triiodothyronine, to have this effect.
Only about 10% of the hormone produced by the gland is T3, which is known as the active thyroid hormone. It’s T3 that is deficient in hypothyroidism and its availability determines the intensity of the metabolic rate.
The large amount of the precursor hormone T4 made the thyroid gland must be converted into T3 by the liver. The liver (if well nourished by a supportive diet and lifestyle) enzymatically converts T4 into T3 as T3 is consumed by the tissues. Most (~70%) of the body’s T3 is provided by the liver, not the thyroid gland.
The liver is an endocrine gland and produces more T3 than does the thyroid! Metabolic slow downs often occur due to poor liver health. Anything that adversely affects liver function will influence metabolism and the production of a majority of the body’s T3. T3 not only determines the intensity of the metabolic rate; but as discussed next, also determines the rate at which cholesterol is converted into steroid hormones and bile salts.
T4, T3, and Cholesterol Metabolism
Thyroid hormones are essential to a healthy metabolism but serve as more than metabolism stimulating hormones. One of their other functions is a role in the conversion of cholesterol into both bile salts and steroid hormones (steroidogenesis).
A thyroid hormone deficiency will thus slow the turnover of cholesterol into bile salts and steroid hormones. The following is a list of factors that contribute to a thyroid hormone insufficiency:
- Polyunsaturated fat rich diet (grains, nuts, seeds, beans, fatty seafood, above ground vegetables, vegetable oils, seed oils, nut butters, fish oils
- Chronic stress
- High adrenaline, cortisol
- Hypoglycemia/Blood sugar dysregulation
- Protein deficiency
- Vitamin/mineral deficiency
- Low red light exposure
- Liver dysfunction
- Excess estrogen
- Radiation
- Progesterone deficiency relative to estrogen
- Over exercise
- Bacterial endotoxin (lipopolysaccharide)
- Low carbohydrate diet
Cholesterol and Metabolism
“A high level of serum cholesterol is practically diagnostic of hypothyroidism, and can be seen as an adaptive attempt to maintain adequate production of the protective steroids. Broda Barnes’ work clearly showed that hypothyroid populations are susceptible to infections, heart disease, and cancer.” -Ray Peat, PhD
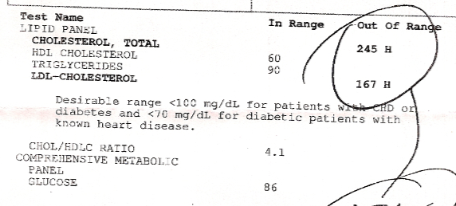
Because thyroid hormone has an established role in steroidogenesis and bile salt synthesis, a thyroid hormone deficiency will lead to a rise in total cholesterol. Accordingly, the hypothyroid typically have high cholesterol while the hyperthyroid typically have low cholesterol. Thyroidectomy (removal of thyroid) results in a rise in serum cholesterol; administration of thyroid restores serum cholesterol levels.
High cholesterol (hypercholesterolemia) can thus serve as a marker of a failing thyroid system. In people over the age of 50, cholesterol has an inverse relationship with mortality. Many studies indicate that in elderly populations low cholesterol is associated with higher risk of all-cause mortality. This serves as an indication of the protective nature of cholesterol and the substances made from it and also is a reflection of the tendency of metabolic rate to decline with age.
An physiologically relevant strategy to decrease high cholesterol would be to assess and correct the underlying factors contributing to the hypothyroid state. The use of T4 and T3 and a thyroid protective diet to facilitate cholesterol’s conversion to other substances may be a consideration. Physiological doses of thyroid hormone to lower cholesterol may not have the accompanying side effects or risks that artificial substances do and have the added benefit of improving metabolic rate.
Slowed cholesterol turnover
This information makes you wonder if the diseases blamed on high cholesterol are not to due cholesterol itself but rather on a failing metabolism and the factors that cause it.
Statin therapy attempts to cut off cholesterol production at the level of the liver without facilitating conversion of cholesterol into steroids or bile salts. Decreasing high cholesterol through conversion into other beneficial substances is a more biologically valuable therapy.
A properly working metabolism allows protective, antioxidant, and anti-inflammatory steroid hormoes such as DHEA, progesterone, and pregnenalone to be made decreasing the likelihood of a variety of disease processes; it also encourages the oxidization of glucose producing ATP, water, and protective CO2; and supports the liver’s production of bile salts responsible for the breakdown of fats and elimination of fat-soluble toxins and excess cholesterol through the bowel.
All in all, the rise of cholesterol in aging and hypothyroidism is not a maladaptive response but a protective one which encourages the synthesis of protective steroids. In a healthy individual, the perpetual turnover of cholesterol in the tissues that occurs when thyroid hormone production is optimal tends to lower the proportion of the toxic oxidized variants of cholesterol while at the same time encouraging the production of protective steroid hormones.
In a chronic hypothyroid state, the conversion of cholesterol to other substances is slowed allowing the toxic oxidized forms of cholesterol to accrue leading to diseases of the cardiovascular system. In this scenario, cholesterol loses its protective functions. Thyroid hormone has been shown to have beneficial effects on those with acute and chronic cardiovascular disease.
Maintain metabolic rate
Nourishing the liver with a constant supply of blood glucose, sufficient protein, and a diet rich in vitamins and minerals will help in the elimination of estrogen and support the conversion of T4 to T3.
Avoiding a high stress lifestyle and hypoglycemic conditions reduces the influence of cortisol and adrenaline, which have multiple adverse affects on the conversion of T4 into T3 production.
Excess estrogen and dietary polyunsaturated fats (PUFA) block the secretion, transport, and action of the thyroid hormone in the tissues. PUFA damage the energy and steroid producing parts of cells, lowering energy production and causing hormone imbalances. PUFA are directly linked with cancer and heart disease progression and are toxic to the liver.
Endotoxin produced in the intestine is a chronic, endogenous stressor that raises estrogen and negatively affects the liver. Bowel regularity decreases the intestinal toxin burden and is paramount to both a healthy liver and a healthy metabolism.
Ripe fruits, milk, orange juice from ripe oranges, honey, sucrose, and well-cooked below ground vegetables provide carbohydrate. Saturated fats and sufficient protein intake that represents consumption of the entire animal would serve to support metabolism and reduce consumption of anti-thyroid substances.
Animal protein is superior to vegetable protein to meet amino acid requirements. Too much animal meat can be anti-thyroid so adults should emphasize gelatin/broth, pastured chicken eggs, milk, and cheese for daily proteins with occasional muscle meat exposures from herbivores along with shellfish for trace minerals, and organ meat once a week for a multivitamin.
Exposure to sunlight improves metabolic function (and affects cholesterol levels) as does living at altitude. Stress reduction has wide sweeping benefits as well because stress impairs thyroid function and affects the blood sugar.
FPS coaches a 12 week nutrition course based on the methodology of Ray Peat, PhD. Please click here for more information.
Resources
(1) “Cholesterol, longevity, intelligence, and health” by Ray Peat, PhD
(2) Blood Cholesterol Values in Hyperthyroidism and Hypothyroidism — Their Significance
http://www.nejm.org/doi/pdf/10.1056/NEJM193012252032601
(3) Dietary cholesterol provided by eggs and plasma lipoproteins in healthy populations.
http://www.ncbi.nlm.nih.gov/pubmed/16340654
It is also important to note that 70% of the population experiences a mild increase or no alterations in plasma cholesterol concentrations when challenged with high amounts of dietary cholesterol (hyporesponders). Egg intake has been shown to promote the formation of large LDL, in addition to shifting individuals from the LDL pattern B to pattern A, which is less atherogenic.
(4) Effects of D- and L-triiodothyronine and of J propylthiouracil on the production of bile acids in the rat
http://www.jlr.org/content/4/3/305.full.pdf
When daily production of bile acids (C + CDC) was calculated from the values of turnover rate and pool size, it was found that normal rats had an average synthesis of 4.9 mg bile acids per day, while the production for the LT3- and DT3-treated rats averaged about 8.0 mg/day. This tendency towards increased total bile acid production in the thyroid hormone-treated rats was mainly due to a 2- to 3-fold increase in the daily synthesis of CDC.
(5) The decrease of liver LDL receptor mRNA during fasting is related to the decrease in serum T3
http://www.ncbi.nlm.nih.gov/pubmed/9608674
In conclusion: (1) Fasting induces a hypothyroid-like condition in which inhibition of hepatic conversion of T4 into T3 may be responsible for the decrease of serum T3. (2) Fasting induces an increase of plasma LDL cholesterol, apparently caused by a decrease of hepatic LDL receptor gene expression which is (partly) related to the fall in serum T3
(6) Effects of L-triiodothyronine and the thyromimetic L-94901 on serum lipoprotein levels and hepatic low-density lipoprotein receptor, 3-hydroxy-3-methylglutaryl coenzyme A reductase, and apo A-I gene expression.
http://www.ncbi.nlm.nih.gov/pubmed/9698096
Thyroidectomy resulted in a 77% increase in plasma LDL cholesterol, a 60% decrease in plasma triglycerides, and a modest reduction in HDL cholesterol. Daily oral dosing with T3 (10-170 nmol/kg) or L94901 (100-1000 nmol/kg) for 7 days decreased plasma LDL cholesterol in thyroidectomized rats by 60-80%, respectively. This reduction in LDL cholesterol was accompanied by a dose-dependent increase in HDL cholesterol levels of up to 60%.
(7) Sterol Balance in Hypothyroidism
http://jcem.endojournals.org/cgi/content/abstract/1/10/799
The onset of thyroid treatment was followed by a marked drop in serum cholesterol of hypothyroid patients. With a daily dose of two grains (128 mg.) of desiccated thyroid the serum cholesterol of patients with hypothyroidism decreased in amounts varying from 117 to 385 mg. per cent (2). When thyroid medication was discontinued the serum cholesterol of patients with hypothyroidism increased greatly in the course of 4 to 20 weeks, reaching levels 98 to 411 mg. per cent above those of the period of treatment in 15 of 17 cases. In normal children the withdrawal of thyroid medication caused an increase of only 10 to 55 mg. per cent (3).
(8) The role of the thyroid in the regulation of the blood cholesterol of rabbits
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2133549/
3. When long continued cholesterol feeding has failed to cause a rise in the blood cholesterol of rabbits, thyroidectomy abolishes this resistance and a hypercholesterolemia is promptly produced. 4. A single injection of thyroxin causes a significant drop in the blood cholesterol of rabbits with hypercholesterolemia. This reaction is not influenced by thyroidectomy.
(9) Cholesterol metabolism in hypothyroidism and hyperthyroidism in man
http://www.jlr.org/content/22/2/323.full.pdf
Treatment of hypothyroid patients produced the expected fall in LDL. One possible mechanism could be that thyroid hormones enhance the conversion of cholesterol into bile acids; this mechanism has been suggested by other workers from animal studies. However, no evidence was obtained in either hypothyroid or hyperthyroid patients that thyroid hormones alter synthesis of bile acids.
(10) Effect of endocrine factors on cholesterol turnover in young and old rats
http://www.ncbi.nlm.nih.gov/pubmed/5111796
(1) Hypophysectomy or thyroidectomy slows down cholesterol turnover in blood and aorta in young rats. Old animals do not react to thyroidectomy and after hypophysectomy only cholesterol turnover in blood is slowed down.
(2) Administration of thyroxine or insulin increases cholesterol turnover in the blood and aorta of the young rats but is without effect in the old rats. A much higher dose of insulin is necessary to increase cholesterol turnover in the blood of old rats.
(3) It is concluded that decrease of cholesterol turnover in old animals can be partly explained by smaller sensitivity of cholesterol metabolism to thyroxine and insulin and by smaller secretion of thyroxine.
(11) Hormonal involvement in the reduction of cholesterol associated with chronic exercise
http://www.springerlink.com/content/w3m72257520j463j/
These findings imply that thyroid hormones are involved in the reduction of cholesterol with exercise.
(12) Function of the hypophysis-thyroid system in the rabbit fetus with regard to cholesterol metabolism
http://chemport.cas.org/cgi-bin/sdcgi?APP=ftslink&action=reflink&origin=npg&version=1.0&coi=1:CAS:528:DyaF3MXkvFKjsA%3D%3D&pissn=0028-0836&pyear=1963&md5=48e92209a910d362e7e5372e02a0c47c
This indicated that the pituitary and thyroid play a part in cholesterol metabolism of the fetus. Apparently, the maternal thyroid hormones and thyrotropic hormone do not compensate for the absence of fetal thyroid and pituitary hormones in the rabbit.
(13) Function of the fetal thyroid of the rabbit with regard to cholesterol metabolism studied by fetal thyroidectomy
http://chemport.cas.org/cgi-bin/sdcgi?APP=ftslink&action=reflink&origin=npg&version=1.0&coi=1:CAS:528:DyaF3MXht1KjtLw%3D&pissn=0028-0836&pyear=1963&md5=94a10863e940ec5aa619bb4131dcbf94
Serum cholesterol levels of thyroidectomized fetuses were significantly higher than those of untreated litter mates, indicating that the fetal thyroid plays a part in fetal cholesterol metabolism.
(14) Seasonal Variation in Serum Cholesterol Levels Treatment Implications and Possible Mechanisms
http://archinte.ama-assn.org/cgi/reprint/164/8/863.pdf
Overall, 22% more participants had total cholesterol levels of 240 mg/dL or greater ( 6.22 mmol/L) in the winter than in the summer.
(15) Serum Cholesterol Variations in Man
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC434849/?page=5
4. Thyroid administration produced a sharp drop in serum cholesterol in every case. This accompanied by a rise in the basal metabolic rate.
(16) Involvement of the steroidogenic acute regulatory (StAR) protein
http://www.jbc.org/content/274/9/5909.full
http://www.jbc.org/content/274/9/5909.full.pdf
The current findings demonstrate for the first time that thyroid hormones, through induction of the SF-1-mediated StAR gene expression, play a major role in the regulation of steroidogenesis.
(17) Interaction of thyroid hormone and steroidogenic acute regulatory (StAR) protein in the regulation of murine Leydig cell steroidogenesis
These findings demonstrate a key role of thyroid hormone in maintaining mouse Leydig cell function, where thyroid hormone and StAR protein coordinately regulate steroid hormone biosynthesis.
(18) Thyroid Hormones: Their role in testicular steroidogenesis
http://informahealthcare.com/doi/abs/10.1080/01485010390204968
Although the role of T3 on sperm, germ, and peritubular cells has not yet been completely studied, it is clear that T3 directly regulates Sertoli and Leydig cell functions. Further studies are required to elucidate the direct effect of T3 on sperm, germ, and peritubular cells.
(19) Leydig cells, thyroid hormones and steroidogenesis.
http://www.ncbi.nlm.nih.gov/pubmed/16313060
It is evident now that thyroid hormones perform many functions in Leydig cells. For the process of postnatal Leydig cell differentiation, thyroid hormones are crucial. Thyroid hormones acutely stimulate Leydig cell steroidogenesis. Thyroid hormones cause proliferation of the cytoplasmic organelle peroxisome and stimulate the production of steroidogenic acute regulatory protein (StAR) and StAR mRNA in Leydig cells; both peroxisomes and StAR are linked with the transport of cholesterol, the obligatory intermediate in steroid hormone biosynthesis, into mitochondria.
(20) Influence of thyroxine on human granulosa cell steroidogenesis in vitro
http://www.springerlink.com/content/u15h32458544423p/
All concentrations of T4 used produced a statistically significant increase in progesterone secretion (range, 1.39 to 1.60 times the baseline amount). The increase in estradiol secretion reached statistical significance only at a T4 concentration of 10–8 M (1.24 times the baseline amount).
(21) The role of thyroid hormone in testicular development and function (review)
http://joe.endocrinology-journals.org/cgi/content/abstract/199/3/351
Thyroid hormone is a critical regulator of growth, development, and metabolism in virtually all tissues, and altered thyroid status affects many organs and systems. Although for many years testis has been regarded as a thyroid hormone unresponsive organ, it is now evident that thyroid hormone plays an important role in testicular development and function. A considerable amount of data show that thyroid hormone influences steroidogenesis as well as spermatogenesis. The involvement of tri-iodothyronine (T3) in the control of Sertoli cell proliferation and functional maturation is widely accepted, as well as its role in postnatal Leydig cell differentiation and steroidogenesis. The presence of thyroid hormone receptors in testicular cells throughout development and in adulthood implies that T3 may act directly on these cells to bring about its effects
(22) Augmentation by thyroxine of human granulosa cell gonadotrophin-induced steroidogenesis
http://humrep.oxfordjournals.org/content/10/11/2845.abstract
All concentrations of thyroxine used produced a statistically significant increase in oestradiol (range 1.18−1.37 times the amount with FSH/LH alone) and progesterone (range 1.29−1.51 times the amount with FSH/LH alone) secretion.
(23) Free thyroid hormones and cholesterol in follicular fluid of bovine ovaries
http://bulletin.piwet.pulawy.pl/archive/50-2/11_Blaszczyk.pdf
Our resultsconfirm that thyroid hormones are required for bovine follicular function and indicate that the intra-follicular concentrations of FT3 and cholesterol may be affected by the season. Our findings suggest that thyroid hormones may be involved in cholesterol metabolism in bovine follicles.
(24) Effect of thyroidectomy on pregnenolone and progesterone biosynthesis in rat adrenal cortex.
http://www.ncbi.nlm.nih.gov/pubmed/7109578
Thyroid hormones may therefore affect the availability of the energy mechanisms connected with the proton motive force, since thyroidectomy reduces both the phosphorylative oxidation and energy-dependent hydroxylation reactions involved in steroidogenesis.
(25) The effect of the treatment of hypothyroidism and hyperthyroidism on plasma lipids and apolipoproteins AI, AII and E.
http://www.ncbi.nlm.nih.gov/pubmed/9059553?dopt=Abstract
Hypothyroidism and hyperthyroidism have opposite effects on plasma lipids and apolipoproteins. In hypothyroidism, total and HDL cholesterol, total/HDL cholesterol ratio, apo AI and apo E are elevated. The increase in apo AI without a concomitant increase in apo AII suggests selective elevation of HDL2. In contrast, hyperthyroidism is associated with decreased total and HDL cholesterol, total/HDL cholesterol ratio, and apo AI levels. These effects are reversible with treatment of the underlying thyroid disorder.
(26) Changes in Plasma Low-Density Lipoprotein (LDL)- and High-Density Lipoprotein Cholesterol in Hypo- and Hyperthyroid Patients Are Related to Changes in Free Thyroxine, Not to Polymorphisms in LDL Receptor or Cholesterol Ester Transfer Protein Genes
http://jcem.endojournals.org/cgi/content/abstract/85/5/1857?ijkey=13f1402d09f6b26242da2f3b06dcd589077fbc41&keytype2=tf_ipsecsha
In conclusion, in the transition from hypo- or hyperthyroidism to euthyroidism, no association is found between AvaII genotype and changes in plasma LDL-C nor between TaqIB genotype and changes in HDL-C. Changes in LDL-C and HDL-C correlate with changes in fT4.
(27) Hypothyroidism: A Double Blind, Placebo-Controlled Trial (Basel Thyroid Study)
http://jcem.endojournals.org/cgi/content/abstract/86/10/4860?ijkey=eb11362f157bc1daa75d5e062644024f1f3b4823&keytype2=tf_ipsecsha
This is the first double blind study to show that physiological L-thyroxine replacement in patients with subclinical hypothyroidism has a beneficial effect on low density lipoprotein cholesterol levels and clinical symptoms of hypothyroidism. An important risk reduction of cardiovascular mortality of 9–31% can be estimated from the observed improvement in low density lipoprotein cholesterol.
(28) The association between TSH within the reference range and serum lipid concentrations in a population-based study. The HUNT Study.
http://www.ncbi.nlm.nih.gov/pubmed/17287407
Within the range of TSH that is considered clinically normal, we found that increasing level of TSH was associated with less favourable lipid concentrations. The association with serum lipids was linear across the entire reference range of TSH.
(29) Effect of Thyroxine Therapy on Serum Lipoproteins in Patients with Mild Thyroid Failure: A Quantitative Review of the Literature
http://jcem.endojournals.org/cgi/content/abstract/85/9/2993
These results, although based on fewer than 250 patients, suggest that T4 therapy in individuals with mild thyroid failure lowers mean serum total and LDL cholesterol concentrations. The reduction in serum total cholesterol may be larger in individuals with higher pretreatment cholesterol levels and in hypothyroid individuals taking suboptimal T4 doses.
(30) Normalization of Hyperhomocysteinemia with L-Thyroxine in Hypothyroidism
http://www.annals.org/content/131/5/348.full.pdf+html
Hypothyroidism may be a treatable cause of hyperhomocysteinemia, and elevated plasma homocysteine levels may be an independent risk factor for the accelerated atherosclerosis seen in primary hypothyroidism
(31) Thyroid Hormone Regulation and Cholesterol Metabolism Are Connected through Sterol Regulatory Element-binding Protein-2 (SREBP-2)
http://darwin.bio.uci.edu/~osborne/DJS1.pdf
In mammals, thyroid hormone depletion leads to decreased LDL receptor expression and elevated serum cholesterol. The clinical association in humans has been known since the 1920s; however, a molecular explanation has been lacking…Thus, we propose that the decreased LDL receptor and increased serum cholesterol associated with hypothyroidism are secondary to the thyroid hormone effects on SREBP-2. These results suggest that hypercholesterolemia associated with hypothyroidism can be reversed by agents that directly increase SREBP-2.
(32) Defects of receptor-mediated low density lipoprotein catabolism in homozygous familial hypercholesterolemia and hypothyroidism in vivo.
http://www.ncbi.nlm.nih.gov/pubmed/6264482
Receptor-mediated catabolism of LDL, determined as the difference between the turnover of 125I and 131I, was found to be virtually absent in two homozygotes with familial hypercholesterolemia and markedly reduced in a hypothyroid patient. Treatment of the latter with L-thyroxine markedly stimulated receptor-mediated catabolism and reduced LDL levels as did cholestyramine administration in a control subject. Reduction of LDL levels by plasma exchange in a control subject and homozygote had no such effect. These results demonstrate the existence of an intrinsic and almost total defect of receptor-mediated LDL catabolism in homozygous familial hypercholesterolemia and demontrate an analogous but reversible abnormality in hypothyroidism.
(33) Cholesterol as risk factor for mortality in elderly women
http://www.ncbi.nlm.nih.gov/pubmed/2564950
The relation between low cholesterol values and increased mortality was independent of the incidence of cancer.
(34) Relationship between plasma lipids and all-cause mortality in nondemented elderly
http://www.ncbi.nlm.nih.gov/pubmed/15673344
Low cholesterol level is a robust predictor of mortality in the nondemented elderly and may be a surrogate of frailty or subclinical disease. More research is needed to understand these associations
(35) Serum total cholesterol levels and all-cause mortality in a home-dwelling elderly population: a six-year follow-up
http://www.ncbi.nlm.nih.gov/pubmed/20470020
Participants with low serum total cholesterol seem to have a lower survival rate than participants with an elevated cholesterol level, irrespective of concomitant diseases or health status.
(36) Lack of association between cholesterol and coronary heart disease mortality and morbidity and all-cause mortality in persons older than 70 years
http://www.ncbi.nlm.nih.gov/pubmed/7772105
Our findings do not support the hypothesis that hypercholesterolemia or low HDL-C are important risk factors for all-cause mortality, coronary heart disease mortality, or hospitalization for myocardial infarction or unstable angina in this cohort of persons older than 70 years
(37) HDL cholesterol predicts coronary heart disease mortality in older persons.
http://www.ncbi.nlm.nih.gov/pubmed/7629981
Low HDL-C predicts CHD mortality and occurrence of new CHD events in persons older than 70 years. Elevated total cholesterol was not found to be associated with CHD mortality in older men, but may be a risk factor for CHD in older women
(38) Low total cholesterol and increased risk of dying: are low levels clinical warning signs in the elderly? Results from the Italian Longitudinal Study on Aging
http://www.ncbi.nlm.nih.gov/pubmed/12834520
Subjects with low TC levels (<189 mg/dL) are at higher risk of dying even when many related factors have been taken into account. Although more data are needed to clarify the association between TC and all-cause mortality in older individuals, physicians may want to regard very low levels of cholesterol as potential warning signs of occult disease or as signals of rapidly declining health
(39) Plasma triglyceride metabolism in thyroid disease.
http://www.ncbi.nlm.nih.gov/pubmed/4341014?dopt=Abstract
There was a significant linear correlation between the concentration and turnover rate of plasma triglycerides in both hyperthyroid and euthyroid subjects but the concentration/turnover rate ratio was less in the former group suggesting that the efficiency of removal of triglycerides from the circulation was improved in thyroid hyperfunction.
(40) Effects of Thyroid Hormone on the Cardiovascular System
http://rphr.endojournals.org/cgi/content/abstract/59/1/31?ijkey=31d707dfeda0c6feea5b673819ea222e4a9e5820&keytype2=tf_ipsecsha
Preliminary clinical investigations suggest that administration of thyroid hormone or its analogue 3,5-diiodothyropropionic acid greatly benefits these patients, highlighting the potential role of thyroid hormone treatment in patients with acute and chronic cardiovascular disease.
(41) The Influence of Age on the Relationship between Subclinical Hypothyroidism and Ischemic Heart Disease: A Metaanalysis
http://jcem.endojournals.org/cgi/content/abstract/93/8/2998
SCH is associated with increased IHD (both prevalence and incidence) and cardiovascular mortality only in subjects from younger populations. These data suggest that increased vascular risk may only be present in younger individuals with SCH.
(42) Subclinical hypothyroidism, arterial stiffness, and myocardial reserve.
http://www.ncbi.nlm.nih.gov/pubmed/16537677
Arterial stiffness was increased in SCH and improved with l-thyroxine, which may be beneficial, whereas myocardial functional reserve was similar to controls and remained unaltered after treatment
(43) Hypothyroidism and Atherosclerosis
http://jcem.endojournals.org/cgi/reprint/88/6/2438.pdf
(44) Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: beneficial effect of levothyroxine therapy.
http://www.ncbi.nlm.nih.gov/pubmed/12915662
Patients with sHT are characterized by endothelial dysfunction resulting from a reduction in NO availability, an alteration partially independent of dyslipidemia and reversed by levothyroxine supplementation.
(45) Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: a double-blind, placebo- controlled study
http://www.ncbi.nlm.nih.gov/pubmed/15126526
L-T(4) replacement significantly reduced both total and LDL cholesterol (P < 0.0001 for both) and mean-IMT (by 11%, P < 0.0001). The decrement in IMT was directly related to the decrements of both total cholesterol and TSH (P = 0.02 and P = 0.0001, respectively). We conclude that early carotid artery wall alterations are present in sHT patients. Whether such IMT increase is related to an early atherosclerotic involvement of the arterial wall cannot be clearly decided on the basis of the present results. However, the fact that L-T(4) replacement therapy was able to improve both the atherogenic lipoprotein profile and intima-media thickening suggests that lipid infiltration of arterial wall may represent a major mechanism underlying IMT increase in subclinical hypothyroidism.
(46) “Altitude and Mortality” by Ray Peat, PhD
(47) High intake of cholesterol results in less atherogenic low-density lipoprotein particles in men and women independent of response classification.
http://www.ncbi.nlm.nih.gov/pubmed/15164336
Because LDL peak diameter was not decreased and the larger LDL-1 subclass was greater in hyperresponders following egg intake, these data indicate that the consumption of a high-cholesterol diet does not negatively influence the atherogenicity of the LDL particle.
(48) Dietary cholesterol does not increase biomarkers for chronic disease in a pediatric population from northern Mexico.
http://www.ncbi.nlm.nih.gov/pubmed/15447890
Intake of 2 eggs/d results in the maintenance of LDL:HDL and in the generation of a less atherogenic LDL in this population of Mexican children.
(49) Pre-menopausal women, classified as hypo- or hyperresponders, do not alter their LDL/HDL ratio following a high dietary cholesterol challenge.
http://www.ncbi.nlm.nih.gov/pubmed/12074253
These data revealed that excess dietary cholesterol does not increase the risk of developing an atherogenic lipoprotein profile in pre-menopausal women, regardless of their response classification. Although the addition of 640 mg of cholesterol to the diet did result in an increase in plasma cholesterol in hyperresponders, the LDL/HDL ratio was maintained.
(50) The effect of thyrotrophic hormone upon serum cholesterol
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1266515/pdf/biochemj01075-0012.pdf
The intraperitoneal injection of the thyrotropic hormone caused a marked
decrease in the serum cholesterol of rats and dogs. The serum cholesterol curve shows a reciprocal relationship to the basal metabolic rate curve of rats receiving chronic injections of the thyrotropic hormone.
(51) Hypothyroidism in coronary heart disease and its relation to selected risk factors
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1994013/
HT was found highly prevalent in patient with clinical coronary heart disease, mainly in females, and was associated with several cardiovascular risk factors.
(52) Thyroid dysfunction and their relation to cardiovascular risk factors such as lipid profile, hsCRP, and waist hip ratio in Korea
http://www.ncbi.nlm.nih.gov/pubmed/14619383
Patients with subclinical hypothyroidism exhibited elevated atherogenic parameters (Total cholesterol, LDL-C). Therefore screening and treatment for subclinical hypothyroidism may be warranted due to its adverse effects on lipid metabolism.
(53) Risk factors for cardiovascular disease in women with subclinical hypothyroidism.
http://www.ncbi.nlm.nih.gov/pubmed/12097204
We conclude that subclinical hypothyroidism in middle-aged women is associated with hypertension, hypertriglyceridemia, and elevated TC/HDL-C ratio. This may increase the risk of accelerated atherosclerosis and premature coronary artery disease in some patients.
(54) Cardiovascular risk factors in patients with subclinical hypothyroidism
http://www.ncbi.nlm.nih.gov/pubmed/18050969
Subclinical hypothyroidism was associated with higher BMI, diastolic hypertension, higher total cholesterol and triglicerides levels and higher total cholesterol/HDL cholesterols ratio. This might increase the risk of accelerated arteriosclerosis in patients with SH.
(55) Thyroid dysfunction and serum lipids: a community-based study
http://www.ncbi.nlm.nih.gov/pubmed/16343102
SCH is associated with increased serum LDL-C concentrations, which is significant after adjustment for age, age(2) and sex.
(56) The effect of L-thyroxine replacement therapy on lipid based cardiovascular risk in subclinical hypothyroidism
http://www.ncbi.nlm.nih.gov/pubmed/15762035
In conclusion, even mild elevations of TSH are associated with changes in lipid profile significant enough to raise the cardiovascular risk ratio, and these changes are corrected once the patients have been rendered euthyroid.
(57) Thyroid substitution therapy induces high-density lipoprotein-associated platelet-activating factor-acetylhydrolase in patients with subclinical hypothyroidism: a potential antiatherogenic effect
http://www.ncbi.nlm.nih.gov/pubmed/15929667
Patients with SH exhibit increased plasma PAF-AH activity and low HDL-associated PAF-AH activity. Levothyroxine induces a significant increase in HDL-PAF-AH activity. This action may represent a potential antiatherogenic effect of thyroid replacement therapy.
(58) Evaluation response and effectiveness of thyroid hormone replacement treatment on lipid profile and function in elderly patients with subclinical hypothyroidism
http://www.ncbi.nlm.nih.gov/pubmed/16621071
It was shown that THR among patients with SCH is beneficial not only by improvement in lipid profile, as well as by improvement in cognitive and functional status, but also in decreasing blood pressure and BMI.
(59) Disturbed lipid metabolism in patients with subclinical hypothyroidism: effect of L-thyroxine therapy.
http://www.ncbi.nlm.nih.gov/pubmed/7949641
Thus, the L-T4 treatment appears to have a preventive effect on the disturbance of lipid metabolism in patients with subclinical hypothyroidism, especially in patients with serum TSH levels above 10 mU/l.
(60) Hypercholesterolemia treatment: a new hypothesis or just an accident?
http://www.ncbi.nlm.nih.gov/pubmed/12445520
A new hypothesis concerning the association of low levels of steroid hormones and hypercholesterolemia is proposed. This study presents data that concurrent restoration to youthful levels of multiple normally found steroid hormones is able to normalize or improve serum total cholesterol (TC). We evaluated 20 patients with hypercholesterolemia who received hormonorestorative therapy (HT) with natural hormones. Hundred percent of patients responded. Mean serum TC was 263.5 mg/dL before and 187.9 mg/dL after treatment. Serum TC dropped below 200 mg/dL in 60.0%. No morbidity or mortality related to HT was observed. In patients characterized by hypercholesterolemia and sub-youthful serum steroid hormones, our findings support the hypothesis that hypercholesterolemia is a compensatory mechanism for life-cycle related down-regulation of steroid hormones, and that broadband steroid hormone restoration is associated with a substantial drop in serum TC in many patients.