Also see:
Universal Principle of Cellular Energy
Carbon Dioxide as an Antioxidant
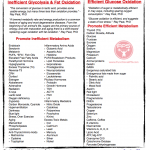
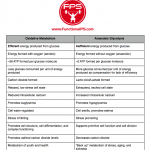
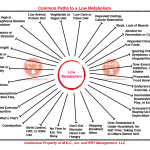
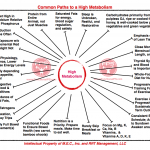
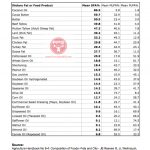
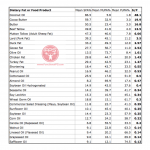
Promoters of Efficient v. Inefficient Metabolism
ATP Regulates Cell Water
Calorie Restriction, PUFA, and Aging
Cardiolipin, Cytochrome Oxidase, Metabolism, & Aging
High Cholesterol and Metabolism
Mitochondria and mortality
Mitochondrial medicine
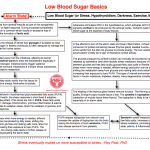
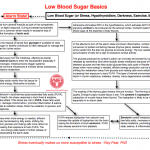
Low Blood Sugar Basics
The Cholesterol and Thyroid Connection
Thyroid Status and Oxidized LDL
The Truth about Low Cholesterol
Hypothyroidism and A Shift in Death Patterns
Light is Right
Using Sunlight to Sustain Life
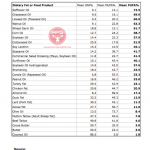
PUFA Decrease Cellular Energy Production
PUFA Breakdown Products Depress Mitochondrial Respiration
“Curing” a High Metabolic Rate with Unsaturated Fats
Power Failure: Does mitochondrial dysfunction lie at the heart of common, complex diseases like cancer and autism?
Faulty Energy Production in Brain Cells Leads to Disorders Ranging from Parkinson’s to Intellectual Disability
Pregnenolone – A Fruit Of Cholesterol
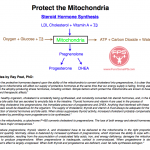
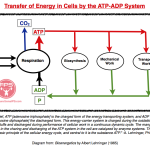
“Mitochondria: small “compartments” in the cytoplasm (the viscous part of the cell, everything but the nucleus), they are responsible for much of the cell’s energy production (as ATP) and oxygen consumption.” -Ray Peat, PhD
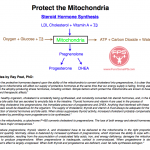
Diagram Inspired by R. Peat and D. Argall
Cellular Energy and Steroid Synthesis
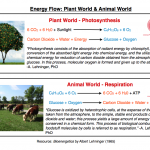
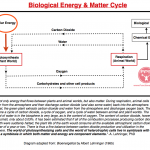
The above chart links two very important concepts – oxidative metabolism and the synthesis of steroid hormones. The cell mitochondrion is the organelle responsible for the production of energy from cellular respiration/oxidative metabolism and steroid hormone synthesis in some cells.
Anything that damages the mitochondria affects the production of energy and the production of protective steroid hormones. Both energy and steroids are needed to handle stress adaptively. A high rate of energy metabolism and continous stream of steroid production is a facet of youthfulness and good health. The opposite occurs in aging and disease.
Dual Role of T3, Toxicity of PUFA
In both the oxidative metabolism and steroid hormone synthesis portions of the chart, please note the dual role of the active thyroid hormone, triiodothyronine (T3), as promoter of cell respiration and co-factor for steroid hormone synthesis. Thyroid hormone also increases the number and size of mitochondria. This make T3 a central figure in stress adaptation. Both the availability of T3 and the health of the mitochondria are partners in the production of energy, synthesis of steroid hormones, and the regulation of cell water.
Dietary polyunsaturates (PUFA) and their toxic breakdown products damage the mitochondria, negatively affect thyroid hormone at multiple points, and interfere with glucose oxidation and the function of important respiratory enzymes (pyruvate dehyrogenase and cytochrome oxidase). These toxic effects of PUFA (impairing energy metabolism & steroid synthesis while increasing oxidative stress & inflammation) make them directly involved in aging, disease processes, and obesity. Saturated fats, or other fats the body formed endogenously from sugar, do not have these effects and are protective.
PUFA Accumulation
As the tissues become more unsaturated with aging or due to poor food choice, the response to stress progressively shifts from adaptive to dysadaptive, making the body increasingly less capable of handling future stresses without producing inflammation and other adverse effects.
The unsaturates’ actions slow the synthesis of youth-promotive steroid hormones (pregnenolone, DHEA, progesterone) from cholesterol, creating a greater reliance on cortisol and increasing the the ratio of estrogen to progesterone. The progressive harm to the mitochondria and respiratory enzymes slows the rate of calorie burn, decreasing the production of energy and carbon dioxide from oxidative metabolism. There is also evidence of degradation of the cytochrome P-450 enzyme, used to form steroids, by lipid peroxides formed from PUFA.
The industrial animal production industry takes advantage of the anti-mitochondria, anti-thyroid, and anti-respiration effects of PUFA by giving animals raised for food production foodstuffs that are high in the polyunsaturates (corn, soy, grain), which fatten the animals cheaply and easily. Polyunsaturates are a component of the western diet now more than ever, fattening the public cheaply and easily.
T3, Respiratory Energy, and CO2
T3 promotes the efficient use of another anti-stress molecule, glucose. In its role of respiration promoter, not only does T3 increase the metabolic rate, but the complete oxidation of glucose produces the “hormone of respiration,” carbon dioxide (CO2), which has many stress-inhibiting and stabilizing functions, including the binding and removal of intracellular calcium that harms the mitochondria.
T3 and Cholesterol Turnover
Cholesterol is another one of the body’s basic protective substances. T3 is needed for cholesterol’s conversion into two other valuable substance: steroid hormones and bile salts. LDL cholesterol’s conversion into pregnenolone by the mitochondrion is of major importance to stress resistance.
Without pregnenolone synthesis, the other protective steroids (like progesterone & DHEA) cannot be made in adequate amounts, increasing the need for cortisol production while simultaneously leaving estrogen unopposed (increased estrogen:progesterone ratio). These consequences are not desirable.
Estrogen, polyunsaturates (PUFA), darkness, iron, radiation, & low cholesterol interfere with the efficiency of this conversion. Thyroid hormone, vitamin A, red light, vitamin E, and copper promote this conversion (see Nutrition for Women by Ray Peat, PhD, Appendix pg. 119).
Cholesterol and Thyroid Connection
The intensity of the metabolic rate has an inverse relationship with cholesterol level. In the first half of the 20th century, elevated serum cholesterol was used as a reliable means to diagnose hypothyroidism. In hypothyroidism (a deficiency of T3), the turnover of cholesterol into protective steroids (and bile salts) decline.
Serum cholesterol increases in hypometabolism due to decreased turnover of cholesterol into steroid hormones and bile salts. The rise of cholesterol in aging and hypothyroidism is not a maladaptive response but a protective one that attempts to encourage the synthesis of protective steroids.
A lack of (red) light or vitamin A (source: beef liver, egg yolks) can contribute to a rise in serum cholesterol and slowed conversion of cholesterol into bile salts and pregnenolone. Conversely, if cholesterol isn’t available in the required amounts, the consequences are similar to when cholesterol is very high – decreased production of pregnenolone, decreased resistance, & steroid hormone imbalance.
Take home points:
1. Mitochondrial health is needed for the respiratory production of energy and carbon dioxide, and steroid hormone synthesis.
2. T3 is needed for the respiratory production of energy and carbon dioxide, steroid hormone synthesis, and bile salt production.
3. Dietary polyunsaturates (PUFA) and their toxic breakdown products damage the mitochondria, negatively affect thyroid hormone at multiple points, and interfere with glucose oxidation and with the function of important respiratory enzymes. Saturated fats, or other fats the body forms naturally from sugar, do not have these effects and are protective.
4. Energy and steroid hormone producing systems fail in the presence of excess food-derived polyunsaturates.
5. The chart in this blog links important concepts: mitochondrial health, thyroid hormone, energy, carbon dioxide, and formation of pregnenolone & other protective steroid hormones. These concepts are central factors in heath v. disease.
Quotes by Ray Peat, PhD:
“In every type of tissue, it is the failure to oxidize glucose that produces oxidative stress and cellular damage.”
“Metabolic energy is fundamental to the development and maintenance of the body, and to the “ways in which living beings react to changed circumstances.” It’s an obvious first thing to consider when thinking about any “disease,” whether it’s cancer, radiation, sickness, dementia, depression, or traumatic injury.”
“The mitochondria are responsible for the efficient production of energy needed for the functioning of complex organisms, and especially for nerves. The enzyme in the mitochondria that reacts directly with oxygen, and that is often rate limiting, is cytochrome oxidase.
This enzyme is dependent upon the thyroid hormone and is inhibited by nitric oxide, carbon monoxide, estrogen, polyunsaturated fatty acids, serotonin, excess or free iron, ionizing radiation, and many toxins, including bacterial endotoxin. Red light, which passes easily through the tissues, reactivates the enzyme, which slowly loses its function during darkness.
Estrogen impairs the mitochondria in multiple ways, including blocking the function of cytochrome oxidase, decreasing the activity of ATP synthase, increasing heme oxygenase which produces carbon monoxide and free iron, damaging mitochondrial DNA, and shifting metabolism from glucose oxidation to fat oxidation, especially by inhibiting pyruvate dehyrogenase complex. These changes including the loss of cytochrome oxidase, are seen in the Alzheimer’s brain. The fact that this kind of energy impairment can be produced by estrogen doesn’t imply that estrogen is the cause, since many other things can cause similar effects–radiation, aluminum, endotoxin, for example.”
“The respiratory activity of the mitochondria declines as the polyunsaturated oils replace palmitic acid, and this change corresponds to the life-long decline of the person’s metabolic rate.”
“All of the nutritional factors that participate in mitochondrial respiration contribute to maintaining a balance between excessive excitation and protective inhibition. Riboflavin, coenzyme Q10, vitamin K, niacinamide, thiamine, and selenium are the nutrients that most directly relate to mitochondrial energy production.”
“The intensity of oxidative metabolism is the basic factor that permits continuing coordination of activity, and harmonious renewal of all the components of the organism.”
“People have spoken of “cascades” in relation to the adrenal glucocorticoids (e.g., cortisol) and estrogen, leading to cell damage, but really both of these hormonal cascades have to be seen as part of a more general collapse of adaptive systems, as a result of both chronic and immediate inadequacies of energy production. ”
“The biochemical details of these cascades are mainly interesting because they show how many different kinds of stress converge on a few physiological processess–mitochondrial energy production, cellular excitation, and intercellular communication–which, when damaged thousands of times, lead to the familiar states of old age. These few functions, damaged by an infinite variety of stresses, have their own complexly adaptive ways of deteriorating, producing the various degenerative diseases.”
“Aging is an energy problem, and in the brain, which has extremely high energy requirements, interference with the energy supply quickly causes cells to die.”
“The presence of carbon dioxide is an indicator of proper mitochondrial respiratory functioning.”
“My argument here will be that some of our adaptive, protective regulatory processes are overridden by the excessive supply of unsaturated fats–supported by a few other toxins–in our diet, acting as a false-signal system, and that cholesterol, pregnenolone, and progesterone which are our main long-range defenses, are overcome by the effects of the unsaturated fats, and that the resulting cascade of ineffective and defective reactions (including various estrogen-stimulated processes) leads to lower and lower energy production, reduced function, and death. At certain times, especially childhood and old age, iron (which also has important regulatory roles) accumulates to the point that its signal functions may be inappropriate.”
“If the internal and external causes of stress converge, additively, on the cell’s internal communication and integration system, then the basic resistance of the organism to stress can be increased by any of the factors which oppose the signals of stress.
Carbon dioxide, progesterone, and thyroid act on many of the factors that interfere with our ability to handle stress constructively. A diet that reduces fermentation and endotoxin, with an abundance of calcium–fruit, milk, and cheese, for example–can help to shift the balance away from lactic acid, estrogen, and serotonin, toward carbon dioxide, progesterone, and thyroid.”
“Carbon dioxide and the major steroids stabilize cells against excessive stimulation, and protect the cell structure.”
“When mitochondria are functioning fully, either glucose or saturated fats can safely
provide energy. Some glucose or saturated fat can be converted to polyunsaturated fats, that can be used as regulators or signals, for example to activate the formation of stem cells. But those PUFA don’t create disruptive cascades of increasing excitation or inflammation or excessive growth, and, from the evidence of animals that are fed fat free diets, or diets lacking omega -3 and omega -6 fatty acids, they aren’t toxic to mitochondria.”
“F. Z. Meerson’s work showed that cortisol, and the free fatty acids mobilized by stress, have a toxic influence on the mitochondrial energy production system. Both cortisol and the free fatty acids block the efficient use of glucose for producing energy, creating a diabetes-like condition.”
“In a variety of cell types, vitamin A functions as an estrogen antagonist, inhibiting cell division and promoting or maintaining the functioning state. It promotes protein synthesis, regulates lysosomes, and protects against lipid peroxidation. Just as stress and estrogen-toxicity resemble aging, so does a vitamin A deficiency. While its known functions are varied, I think the largest use of vitamin A is for the production of pregnenolone, progesterone, and the other youth-associated steroids. One of vitamin E’s important functions is protecting vitamin A from destructive oxidation. Although little attention has been given to the effects of unsaturated fats on vitamin A, their destruction of vitamin E will necessarily lead to the destruction of vitamin A. The increased lipid peroxidation of old age represents a vicious circle, in which the loss of the antioxidants and vitamin A leads to their further destruction.”
“When a muscle or nerve is fatigued, it swells, retaining water. When the swelling is extreme, its ability to contract is limited. Excess water content resembles a partly excited state, in which increase amounts of sodium and calcium are free in the cytoplasm. Energy is needed to eliminate the sodium and calcium, or to bind calcium allowing the cell to extrude excess water and return to the resting state. Thyroid hormone allows cells’ mitochondria to efficiently produce energy, and it also regulates the synthesis of proteins (phospholamban and calcisequestrin) that control the binding of calcium. When the cell is energized, by the mitochondria working with thyroid, oxygen, and sugar, these proteins change their form, binding calcium and removing it from the contractile system, allowing the cell to relax, to be fully prepared for the next contraction. If the calcium isn’t fully and quickly bound, the cell retains extra water and sodium, and isn’t able to fully relax.”
“The mitochondria, by their ability to use oxygen, are responsible for the normal efficient use of glucose.
Beginning at sunset, darkness progressively damages mitochondria structurally and functionally. Mitochondrial damage, and the functional impairment of organs such as the heart muscle, reach a peak at dawn.
During the day (in organisms which survive the night), mitochondrial structure is restored, and organ function improves, with the peak being reached at sunset. In winter, there is cumulative damage to mitochondria, because of too few daylight hours to complete the rebuilding of mitochondria. During the summer (in organisms that live long enough) the cumulative damage is mostly repaired.
A residue of altered cell and tissue structure, and of impaired enzyme function, remains under natural conditions of day-night cycles.”
“The arguments I have outlined for considering rosacea to be essentially a problem of metabolic energy, and the mechanisms that I mention for restoring mitochondrial functions, might seem more complex than Hoffer’s orthomolecular views. However, this approach is actually much simpler conceptually than any of the ideologies of drug treatment. It simply points out that certain excitatory factors can interfere with energy production, and that there are opposing “inhibitory” factors that can restore energy efficiency. Sometimes, using just one or two of the factors can be curative.
Because mitochondrial respiration is very similar in every kind of tissue, a physiological view of rosacea could incline us toward considering the effects of these metabolic factors in other organs during stress and aging–what would the analogous condition of rosacea and rhinophyma be in the brain, heart, liver, or kidney?”
“In the Randle effect (it’s called the “Randle cycle,” but there is no cycle), increasing the amount of fat in the bloodstream decreases the ability of cells to metabolize glucose; glucose tolerance decreases, as in diabetes, except that the response to fat is instantaneous. Respiration decreases, mitochondria retain calcium, which tends to accumulate until it destroys the mitochondria. The calcium, when it is released from the mitochondria, causes excitation to increase. Stimulation without efficient energy production leads to proteolysis and apoptosis or other forms of cell death. Sugars replace carbon dioxide and acetate on lysines. This process is involved in diabetes, Alzheimer’s disease, arthritis, and other degenerative diseases, probably including osteoporosis. Mitochondrial damage tends to increase the production of lactic acid instead of carbon dioxide, and lactic acid can stimulate the inappropriate overgrowth of blood vessels, as occurs in the eyes in diabetes. During stress and aging, free fatty acids appear in the bloodstream in large quantities.”
“While Arthur Everitt, Verzar, and others were studying the effects of the rat’s pituitary (and other glands) on collagen, W. D. Denckla investigated the effects of reproductive hormones and pituitary removal in a wide variety of animals, including fish and mollusks. He had noticed that reproduction in various species (e.g., salmon) was quickly followed by rapid aging and death. Removing the pituitary gland (or its equivalent) and providing thyroid hormone, he found that animals lacking the pituitary lived much longer than intact animals, and maintained a high metabolic rate. Making extracts of pituitary glands, he found a fraction (closely related to prolactin and growth hormone) that suppressed tissue oxygen consumption, and accelerated the degenerative changes of aging…A high level of respiratory energy production that characterizes young life is needed for tissue renewal. The accumulation of factors that impair mitochondrial respiration leads to increasing production of stress factors, that are needed for survival when the organism isn’t able to simply produce energetic new tissue as needed. Continually resorting to these substances progressively reshapes the organism, but the investment in short-term survival, without eliminating the problematic factors, tends to exacerbate the basic energy problem. This seems to be the reason that Denckla’s animals, deprived of their pituitary glands, but provided with thyroid hormone, lived so long: they weren’t able to mobilize the multiple defenses that reduce the mitochondria’s respiratory energy production.”
“W.D. Denckla’s version of programmed aging proposed that the pituitary gland was the agent of this programmed aging. He based his idea on the observation that when animals were kept on a semi-starvation diet, starting before puberty, their puberty was delayed and they lived longer than normal, and on later studies showed that when animals’ pituitary glands were removed before puberty, they lived much longer than normal, and all of their tissues and systems aged at a much slower rate. The implication was that if the gland is present and causes aging, its evolutionary purpose is to cause aging, as well as the other process such a reproduction.
The particular function that Denckla focused on as an index of aging was oxygen consumption, which decreases by more than 70% between puberty and old age. He showed that the decrease of oxygen consumption was much less when the pituitary gland was removed, if the animal was given the amount of thyroid hormone that it would normally produce. He found fairly specific pituitary extracts that decreased oxygen consumption, inhibiting the effects of the thyroid hormone, but he never identified a particular pituitary hormone as the antirespiratory aging hormone, or the mechanism responsible for the extract’s effects.”
“The suppressive effects of unsaturated fats on mitochondrial energy production have been widely investigated, since it is that effect that makes animal fattening with PUFA so economical. Rather than interpreting that as a toxic effect, using the innate structure and function of the mitochondrion as a point of reference from which to evaluate dietary components, the consumption of “good” oils is being used as the reference point from which to evaluate the meaning of metabolism (“efficiency is good,” “low oxygen consumption is good”). Building on the idea that the oils are health-promoters which increase metabolic efficiency, the never-viable “rate of aging” theory was resuscitated: The anti-respiratory effect of PUFA is used (illogically) to return to the idea that aging occurs in proportion to the amount of oxygen consumed, because animals which lack the supposedly essential nutrients (“defective animals”) consume oxygen rapidly–burning calories rapidly, they are supposed to be like a candle that won’t last as long if it burns intensely. The old theory is simply resuscitated to explain why the anti-respiratory action of PUFA might be beneficial, justifying further promotion of their use as food and drugs.”
“The reason for the menopausal progesterone deficiency is a complex of stress-related causes. Free-radicals (for example, from iron in the corpus luteum) interfere with progesterone synthesis, as do prolactin, ACTH, estrogen, cortisol, carotene, and an imbalance of gonadotropins. A deficiency of thyroid, vitamin A, and LDL-cholesterol can also prevent the synthesis of progesterone. Several of the things which cause early puberty and high estrogen, also tend to work against progesterone synthesis. The effect of an intra-uterine irritant is to signal the ovary to suppress progesterone production, to prevent pregnancy while there is a problem in the uterus. The logic by which ACTH suppresses progesterone synthesis is similar, to prevent pregnancy during stress. Since progesterone and pregnenolone protect brain cells against the excitotoxins, anything that chronically lowers the body’s progesterone level tends to accelerate the estrogen-induced excitotoxic death of brain cells.”
“When mitochondria are “uncoupled,” they produce more carbon dioxide than normal, and the mitochondria produce fewer free radicals. Animals with uncoupled mitochondria live longer than animals with the ordinary, more efficient mitochondria, that produce more reactive oxidative fragments. One effect of the high rate of oxidation of the uncoupled mitochondria is that they can eliminate polyunsatured fatty acids that might otherwise be integrated into tissue structures, or function as inappropriate regulatory signals.”
“The regulation of cell renewal probably involves all of the processes of life, but there are a few simple, interacting factors that suppress renewal. The accumulation of polyunsaturated fats, interacting with a high concentration of oxygen, damages mitochondria, and causes a chronic excessive exposure to cortisol. With mitochondrial damage, cells are unable to produce the progesterone needed to oppose cortisol and to protect cells.
Choosing the right foods, the right atmosphere, the right mental and physical activities, and finding the optimal rhythms of light, darkness, and activity, can begin to alter the streaming renewal of cells in all the organs. Designing a more perfect environment is going to be much simpler than the schemes of the genetic engineers. “
“Unsaturated oil tends to lower the blood sugar in at least three basic ways. It damages mitochondria, causing respiration to be uncoupled from energy production, meaning that fuel is burned without useful effect.”
“Progesterone, because of its normal anesthetic function (which prevents the pain of childbirth when its level is adequate), directly quiets nerves, and in this way suppresses many of the excitotoxic processes. It has direct effects on mitochondria, promoting energy production, and it facilitates thyroid hormone functions in various ways.”
“The skeletal changes (shrinkage, curving of the back, moving forward of the lower jaw) which are so characteristic of old age in humans, also occur in other animals in aging and under the influence of the stress hormones. Since the protective hormones depend on the ability of mitochondria to convert cholesterol into pregnenolone, it is clear that damage to mitochondria will affect our supply of protective hormones at the same time that our energy supply is failing, forcing us to shift to the atrophy producing stress hormones, including cortisol. Simple factors which protect the mitochondria are known to have profound therapeutic effects. At a certain point, I think we will understand mitochondrial protection well enough to prevent and cure the basic pathologies of aging. The Mayans and Eskimos studied by Crite produced 25% more biologicaJ energy at rest than people in the U.S. and Europe. They are culturally and nutritionally very different from each other, but they have enough in common to make them very different metabolically from the Euro-American culture. What they have in common is possibly something as simple as the absence of thyroid-inhibiting substances
in their diet.”
“Environmental enrichment, learning, high altitude, and thyroid hormone promote the formation of new mitochondria, and stimulate stem cell proliferation.”
“When we talk about increasing the metabolic rate, and the benefits it produces, we are comparing the rate of metabolism in the presence of thyroid, sugar, salt, and adequate protein to the “normal” diet, containing smaller amounts of those “stimulating” substances. It would be more accurate if we would speak of the suppressive nature of the habitual diet, in relation to the more optimal diet, which provides more energy for work and adaptation, while minimizing the toxic effects of free radicals.”
“The suppression of mitochondrial respiration increases the production of toxic free radicals, and the decreased carbon dioxide makes the proteins more susceptible to attack by free radicals.”
“Pregnenolone is known to be produced (in the mitochondria) from cholesterol. This is the first stage in the production of all of the steroid hormones. If pregnenoione synthesis is insufficient, supplementary pregnenolone would help to maintain an optimum level of the various other steroids. Aging,stress, depression, hypothyroidism, and exposure to toxins are conditions in which synthesis of pregnenolone might be inadequate.”
“High cholesterol is more closely connected to hypothyroidism than hypertriglyceridemia is. Increased T3 will immediately increase the conversion of cholesterol to progesterone and bile acids. When people have abnormally low cholesterol, I think it’s important to increase their cholesterol before taking thyroid, since their steroid-forming tissues won’t be able to respond properly to thyroid without adequate cholesterol.”
“The brain is the body’s richest source of cholesterol, which, with adequate thyroid hormone and vitamin A, is converted into the steroid hormones pregnenolone, progesterone, and DHEA, in proportion to the quantity circulating in blood in low-density lipoproteins. The brain is also the richest source of these very water-insoluble (hydrophobic) steroid hormones; it has a concentration about 20 times higher than the serum, for example. The active thyroid hormone is also concentrated many-fold in the brain.
DHEA (dehydroepiandrosterone) is known to be low in people who are susceptible to heart disease or cancer, and all three of these steroids have a broad spectrum of protective actions. Thyroid hormone, vitamin A, and cholesterol, which are used to produce the protective steroids, have been found to have a similarly broad range of protective effects, even when used singly.”
“Calcium, which is released into the cytoplasm by the excitotoxins, triggers the release of fatty acids, the activation of nerve and muscle, and the release of a variety of transmitter substances, in a cascade of excitatory processes, but at the same time, it tends to impair mitochondrial metabolism, and progressively tends to accumulate in mitochondria, leading to their calcification death, which is also promoted by the antirespiratory effects of the unsaturated fatty acids and the lipid peroxidation they promote. Iron and calcium both tend to accumulate with aging or stress, and both promote excitatory damage; bicarbonate contributes to keeping iron in its inactive state, and probably has a similar effect against a broad spectrum of excitatory substances. Histamine release, nitric oxide, and carbon monoxide are broadly involved in excitotoxic damage, and carbon dioxide tends to be protective against these, too.”
“Estrogen blocks the release of hormone from the thyroid gland, and progesterone facilitates the release. Estrogen excess or progesterone deficiency tends to cause enlargement of the thyroid gland, in association with a hypothyroid state. Estrogen can activate the adrenals to produce cortisol, leading to various harmful effects, including brain aging and bone loss. Progesterone stimulates the adrenals and the ovaries to produce more progesterone, but since progesterone protects against the catabolic effects of cortisol, its effects are the opposite of estrogen’s. Progesterone has antiinflammatory and protective effects, similar to cortisol, but it doesn’t have the harmful effects. In hypothyroidism, there is a tendency to have too much estrogen and cortisol, and too little progesterone.
The blood tests can be useful to demonstrate to physicians what the problem is, but I don’t think they are necessary. There is evidence that having 50 or 100 times as much progesterone as estrogen is desirable, but I don’t advocate “progesterone replacement therapy” in the way it’s often understood. Progesterone can instantly activate the thyroid and the ovaries, so it shouldn’t be necessary to keep using it month after month. If progesterone is used consistently, it can postpone menopause for many years.
Cholesterol is converted to pregnenolone and progesterone by the ovaries, the adrenals, and the brain, if there is enough thyroid hormone and vitamin A, and if there are no interfering factors, such as too much carotene or unsaturated fatty acids. Progesterone deficiency is an indicator that something is wrong, and using a supplement of progesterone without investigating the nature of the problem isn’t a good approach. The normal time to use a progesterone supplement is during the “latter half” of the cycle, the two weeks from ovulation until menstruation. If it is being used to treat epilepsy, cancer, emphysema, migraine or arthritis, or something else so serious that menstrual regularity isn’t a concern, then it can be used at any time. If progesterone is used consistently, it can postpone menopause for many years.”